Since 2019, different industries across Japan have begun implementing upper limit regulations on overtime and holiday working hours under the “Work Style Reform Act.” A five-year grace period was given to the medical industry, with the Revised Medical Law enacted in 2021. After three years of preparation, overtime and holiday working for doctors will be limited from April 1 this year to no more than 960 hours a year, with some exceptions depending on the type of medical institution. What changes will this bring about for physicians working in the clinical field and what does it mean for those of us using the medical system?
In this edition of the COSMO newsletter, we take a closer look at issues facing the medical industry in 2024 and how to respond to them, with input from Dr. Jun Itami of Shin-Matsudo Central General Hospital. Read on to the end for Dr. Itami’s full profile.
Medical practices propped up by long working hours
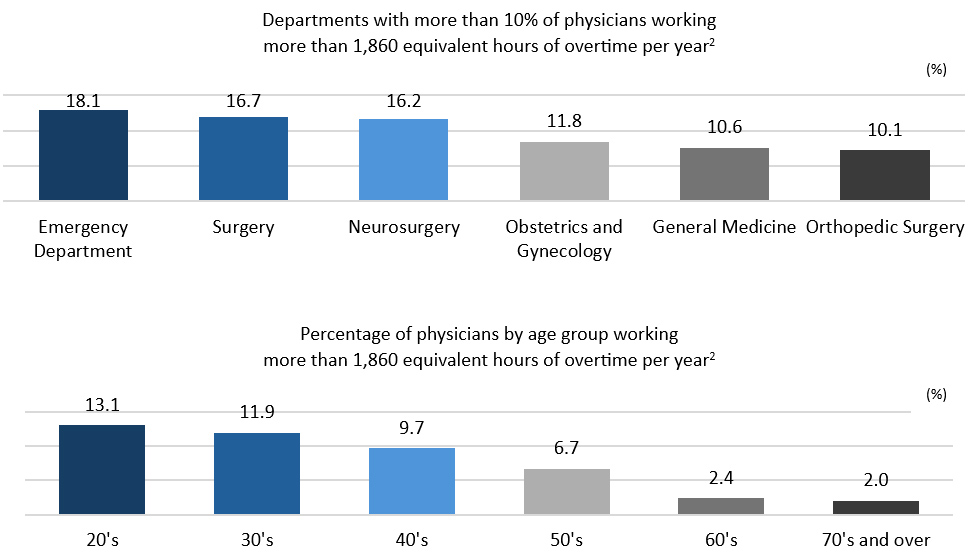
First, let’s take a look at data from the Ministry of Health, Labour and Welfare (MHLW) to understand the work conditions that medical practitioners are typically experiencing. Around 40% of full-time hospital physicians currently work more than 960 hours per year, and another 10% work more than 1,860 hours per year on overtime and during holidays.1 According to an MHLW report2, overtime hours vary by department, with emergency departments, surgery, neurosurgery, obstetrics and gynecology having a particularly high percentage of physicians engaged in long overtime hours. The burden is higher among younger generations, but a number of physicians in their 40s and 50s are also working long overtime hours. (See graph below).
Working long hours doesn’t just damage physicians’ health, it also affects the quality of medical care they provide to patients. A study group on the work style reforms for doctors confirmed that “brain function declines after long hours of continuous work or all-nighters.”2 Accumulated fatigue due to lack of sleep has also been shown to decrease ethical awareness. Cases of physicians choosing to commit suicide due to extreme stress have also been reported, with this topic now becoming a major social problem.
Doctors’ overtime and holiday working hours limited to 960 hours per year
The work style reforms for doctors has come about in response to this situation. The revised Medical Service Act will be fully implemented this spring, with an aim of reducing overtime work in order to ensure the physical and mental health of doctors, as well as providing high-quality medical care in a sustainable manner. Under the law, overtime and holiday work limits for physicians will be set for each type of medical institution, and it will become mandatory for physicians to allocate time for interview assessments (where doctors check their health condition), and rest periods. (See table below).
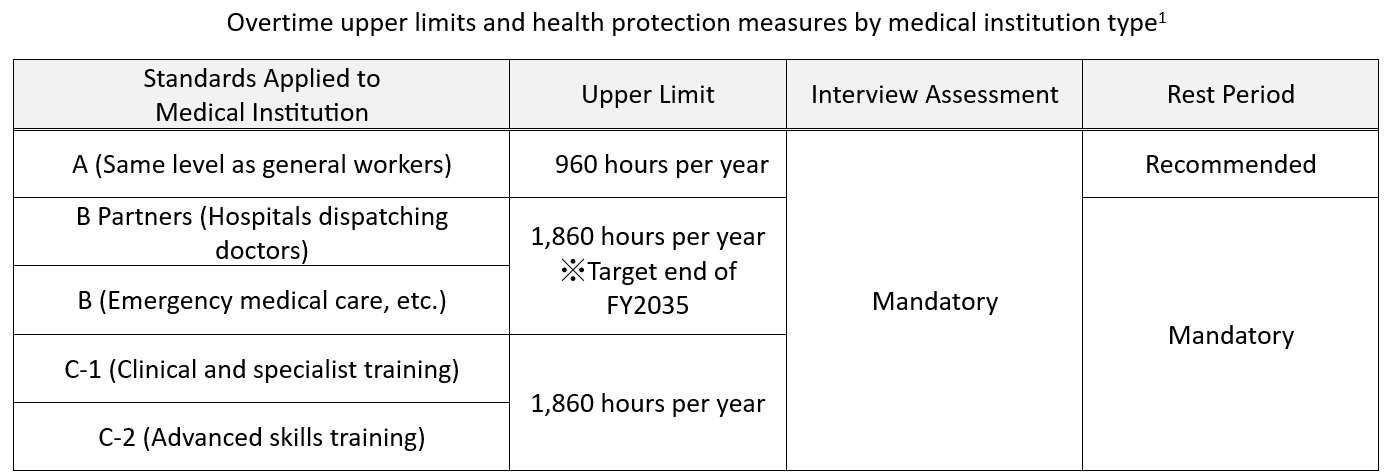
As a result, overtime and holiday working hours for general practitioners (A) will be capped at 960 hours a year. However, as a time-limited measure until the end of fiscal 2035, the upper limit will be 1,860 hours per year for hospitals that dispatch doctors (university hospitals, etc.) and designated medical institutions (B Partners and B). This same limit of 1,860 hours per year will also apply to clinical, specialist and advanced skills training facilities (C-1 and C-2). For these institutions it’s not a time-limited measure, but the ultimate goal is still to reduce the number of hours, with all medical institutions required to aim for “no more than 960 hours per year” of overtime and holiday work in the future.
Restrictions on dispatch doctors supporting local medical services
It would be a welcome development if these limits free physicians from working long hours while at the same time fostering a medical system that can provide high quality medical care. However, the issue behind the long working hours still persists—a shortage of doctors in regional medical care. This leaves some concerned that it will bring about various strains for the industry.
Dr. Jun Itami, Director of the Shin-Matsudo Accuracy Radiation Therapy (SMART) Center at Shin-Matsudo Central General Hospital says, “The medical field requires a large number of doctors for outpatient and on-duty care, and many doctors dispatched from university hospitals are currently supporting the medical field in a dual role. However, restrictions to doctors’ working hours may make it impossible for university hospitals to dispatch doctors in the future.”
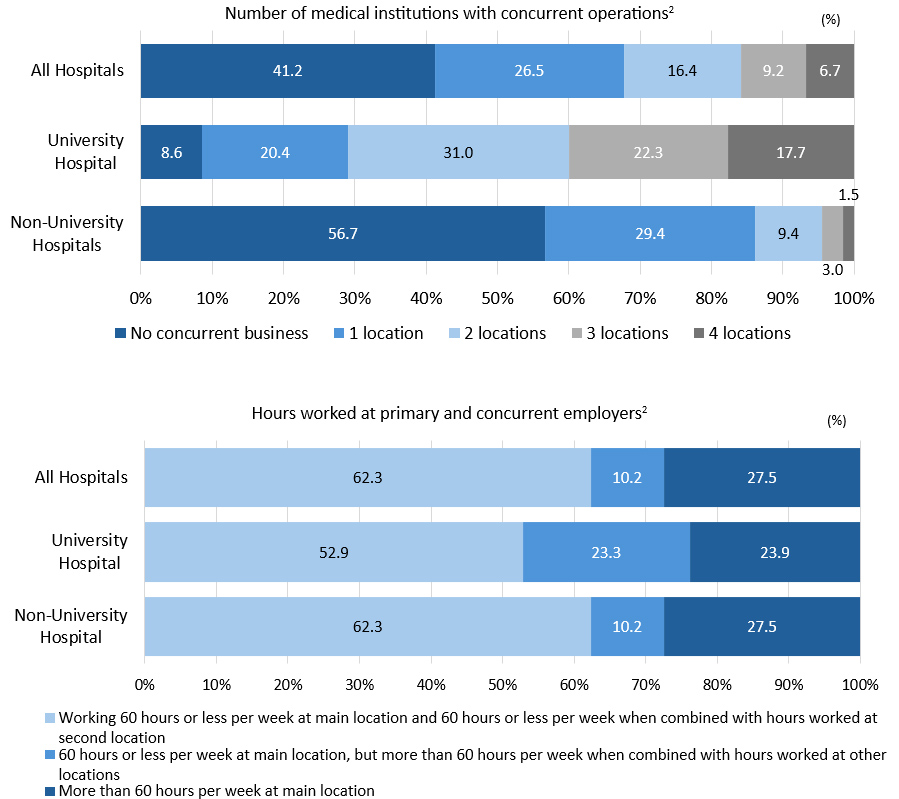
The dispatch of physicians is prohibited under the Worker Dispatch Act,3 but an exception is made for dispatch workers in remote areas or at facilities where it is deemed “necessary to assign dispatch workers to ensure regional medical care.” In the afore-mentioned MHLW report,2 more than 90% of full-time physicians at university hospitals were working concurrently at other medical institutions. The report shows that half of the full-time physicians at university hospitals worked more than 60 hours per week (equivalent to 960 hours of overtime and holiday work per year), and half of them worked more than 960 hours per year when combined with overtime and holiday work at their dual jobs. These figures clearly show that Japan’s regional medical services are supported by dispatch workers (especially full-time university physicians) working concurrently. (See graph below).
Additionally, according to a survey report by the National University Hospital Council of Japan5, national universities across the country dispatched doctors to approximately 10,000 hospitals. Most of these were sent to hospitals within the same prefecture as the national university, but there were some cases where doctors were dispatched to a different prefecture. For the time being, national universities intend to continue dispatching doctors using the “B Partners” system, but this is a temporary measure due to end soon. As such there remains a need for a fundamental solution to solve this issue of a shortage of doctors in local medical care.
Risk of serious impact such as limiting emergency services and capping patients
How will these work style reforms for doctors affect those of us using medical institutions? Dr. Itami fears that the difficulty in dispatching physicians from university hospitals “may lead to serious issues, such as a reduction in emergency services and a cap on the number of patients.” This is owing to the fact that many hospitals are in short supply of physicians, and particularly national and public hospitals are also experiencing difficulty finding replacement physicians if, for example, required to cover those on maternity leave. The number of on-duty physicians may also be reduced, and Dr. Itami is concerned that, in some cases, this may mean hospitals cannot accept ambulances if there is no doctor on duty.
A number of efforts have been launched in response in an effort to maintain local medical services. While encouraging medical institutions to adopt appropriate labor management, the MHLW has also launched a dedicated Japanese-language website6 designed to educate end users about how best to use family doctors, emergency medical care, and telephone consultations (#8000 for issues concerning children and #7119 for adults). University hospitals across Japan have also begun efforts to optimize their medical care systems by promoting referrals to family doctors (reverse referrals), reviewing consultation hours and days of the week, and encouraging patients to see a doctor on the day of their first appointment as much as possible.5
It’s time for all stakeholders to think and act towards realizing a sustainable healthcare system
The shortage of physicians supporting the medical system is not something that can be solved overnight. Dr. Itami proposes specific measures, including “increasing compensation for physicians in medical specialties where the number of physicians is small and the workload is heavy; creating an environment where female physicians can easily return to work after maternity leave; and expanding opportunities for nurses and medical secretaries to play more active roles.”
The report also suggests that work style reform for doctors represents an opportunity for all stakeholders, including the general public, to become more aware of current issues facing the medical field. We should all be thinking about we can do from our respective standpoint and take action to help solve the problems. The healthcare industry is naturally deeply involved in the front lines of medicine and healthcare administration and well versed in the field of communication with patients. In this respect it can also play a role in realizing the ultimate work style reform for doctors, which is to realize a sustainable healthcare system. Multi-stakeholder cooperation will be essential if Japan is to maintain its world-class, high-quality healthcare system for the future.
| Profile: Dr. Jun Itami Director, Shin-Matsudo Accuracy Radiation Therapy (SMART) Center, Shin-Matsudo Central General Hospital Germany. In 2015, he was appointed as a Guest Professor at Chiba University, and has served as Executive Officer of Radiation Protection and Safety at the International Medical Center of Japan, Executive Officer of Radiation Protection and Safety at the National Cancer Center Hospital, and Professor at the Nagasaki University School of Medicine Comprehensive Oncology. He has held his current position since 2021. Dr. Itami is certified in radiation therapy by the Japan Radiological Society and in neutron capture therapy by the Japanese Society of Neutron Capture Therapy. |
 |
References and more information
Ministry of Health, Labour and Welfare, “Doctors’ Workplace Reform.jp”
https://iryou-ishi-hatarakikata.mhlw.go.jp
Ministry of Health, Labour and Welfare, “Let’s learn by cartoon! Reform of the way doctors work”
https://iryou-kinmukankyou.mhlw.go.jp/manga
1) Ministry of Health, Labour and Welfare: “Work Style Reforms for Doctors”, (Japanese only)
https://www.mhlw.go.jp/content/10800000/001129457.pdf
2) Ministry of Health, Labour and Welfare: “The Actual Working Conditions of Doctors” (September 30, 2020),(Japanese only)
https://www.mhlw.go.jp/content/10800000/000677264.pdf
3) Ministry of Health, Labour and Welfare: “Minutes of the 5th Study Group on Work Style Reform for Doctors” (December 22, 2017), (Japanese only)
https://www.mhlw.go.jp/stf/shingi2/0000191239.html
4) Ministry of Health, Labour and Welfare: “Businesses prohibited from using dispatch workers”, (Japanese only)
https://www.mhlw.go.jp/file/06-Seisakujouhou-11600000-Shokugyouanteikyoku/0000133886.pdf
5) National University Hospital Council of Japan Press Conference (May 19, 2020), (Japanese only)
http://nuh-forum.umin.jp/report/kaigi/pdf/230519.pdf
6) Ministry of Health, Labour and Welfare website with advice on how to receive good medical care: (Japanese only)
https://kakarikata.mhlw.go.jp
■Previous COSMO PR Newsletters
●The Year in Review & Optimism for 2024
https://cosmopr.co.jp/en/the-year-in-review-optimism-for-2024-en/
●Health Care and The Environment: The Risks Posed by Climate Change
https://cosmopr.co.jp/ja/climate-change-en/
●Healthcare and the Environment: Understanding the Movement around PFAS
https://cosmopr.co.jp/ja/healthcare-and-the-environment-en/
●Solving Challenges Around Rare and Intractable Diseases Through Stakeholder Collaboration
https://cosmopr.co.jp/ja/solving-challenges-around-rare-en/
●Women’s mental health advice from a medical practitioner in the field: The importance of creating a supportive atmosphere for those experiencing mental health issues
https://cosmopr.co.jp/ja/womens-mental-health-advice-en/
●The current state of women’s mental health in Japan: How should we respond to deepening challenges brought about by the pandemic?
https://cosmopr.co.jp/ja/the-current-state-of-womens-mental-health-in-japan-en/
●Spotlight on Women’s Health in Japan:The role of femtech in the lives of women
https://cosmopr.co.jp/ja/womens-health-in-japan-en/