The impact of ePRO on patients’ cancer treatment experience
-Benefits and issues of ePRO as observed in real-word clinical settings-
Cosmo Public Relations (“COSMO”) and Welby, Inc. co-sponsored an online seminar on May 21, 2021 titled: “The impact of ePRO on patients’ cancer treatment experience: the benefits and issues of ePRO as observed in real-world clinical settings.”
The event brought together professionals committed to exploring the use of new digital solutions to improve the treatment experience of patients with cancer, as well as learning about the potential of such tools to strengthen communication between healthcare providers and patients. We learned that:
- Patients who live in remote areas often delay treatment for adverse reactions due to geographical distance.
- Patients have also delayed treatment due to the COVID-19 pandemic.
- ePRO can enhance remote patient monitoring.
- There was improvement in the accuracy of symptom assessment and enhancement of communication between healthcare providers and patients.
- The tool can be difficult to use with those who may be less familiar with smartphone apps and digital tools.
- Survey results revealed that there are more medical professionals than patients who do not fully understand the benefits of ePRO.
- Successful implementation of ePRO requires careful coordination between all relevant parties.
COSMO Senior Account Director Yuka Kayashima kicked off the event with an introduction to the results from the company’s patient insight survey* conducted on 300 patients in 2020: “The biggest concern of patients receiving cancer treatment was adverse reactions, rather than the effectiveness of the treatment. Particularly notable was the fact that greater numbers of patients with women’s cancers expressed concerned about adverse reactions than patients with cancer overall by 10-30 points, reflecting how much value is placed on maintaining quality of life (QOL). The clinical use of electronic patient-reported outcomes (ePRO), which we will be highlighting today, may serve as a means to help such concerned and struggling patients with cancer consider and continue treatment in a positive light.”
*Visit here for details of COSMO’s Patient Insight Reports on patients with cancer and patients with women’s cancers, including how to purchase.
Akihito Iokawa, Executive Officer, Head of Medical Solution Division of Welby, Inc., a company offering personal health record (PHR) services for patients with cancer, highlighted aspects of PHR, including its structure, advantages for patients, healthcare providers and pharmaceutical companies, and future potential impact.
Participants heard from two keynote speakers: Tetsuhiko Taira, Director, Department of Oncology at Sagara Hospital (Kagoshima Prefecture), who currently uses ePRO in a clinical setting, and Tempei Miyaji, Project Assistant Professor at The University of Tokyo, who conducts research on the latest ePRO in the oncology area. The seminar capped off with a panel discussion and Q&A session on the issues and potential of digital tools for managing patients’ conditions. Those who attended were able to further their understanding of the latest information and emerging issues surrounding ePRO, and consider the future of digital solutions.
Summaries and digests of both presentations follow below.
Click here to access the video of the presentations, panel discussion, and Q&A (Japanese language only).
Summary
In May 2020, Sagara Hospital in Kagoshima City implemented PHR for patients with breast cancer. Tetsuhiko Taira explained that the hospital believed it needed to reinforce its management of adverse reactions. Patients who live in remote regions or on remote islands often delay treatment of adverse reactions due to their geographical location, and maintaining their general treatment at effective levels proved to be a challenge. At the same time, there was also concern for other patients who refrained from visiting the hospital due to the COVID-19 pandemic.
A year has passed since the hospital implemented ePRO. While most patients expressed appreciation for ePRO, with many citing a sense of security being connected to the hospital, other patients pointed out that several questions were irrelevant to their particular set of adverse reactions, adding that if the questions were more relevant to them, it would have prompted them to check their own condition more accurately, which in turn would have served as valuable information for their doctors.
Tempei Miyaji shared research results and data to describe how the use of ePRO is gaining momentum. Explaining how the benefits of ePRO is garnering attention in respective countries, he emphasized the need to improve accuracy of symptom assessments. One way to do this is to incorporate patient assessments. He further pointed out, “As the actual use of ePRO progresses, issues are starting to surface. When implementing it at clinical sites, strategies need to be developed in light of inhibitors and success factors identified by research.” Meanwhile, on the future of ePRO, he forecasts, “ePRO will likely progress not wholly on its own, but rather, in combination with online healthcare, mHealth (mobile health) technologies, and patient portals.”
Digest
Presentation 1
How PHR can transform disease management for patients with cancer
-The potential of self-management as observed in a clinical setting-
Tetsuhiko Taira, Director, Department of Oncology and Director, Clinical Research Center at Sagara Hospital
Background of ePRO implementation
Sagara Hospital’s efforts to implement ePRO began in 2019, when the hospital developed its own electronic self-care forms to gauge if patients receiving anti-cancer therapies were experiencing adverse reactions. To examine the effectiveness of the electronic self-care forms, we asked 20 patients to make entries in both the electronic form as well as print-based form. Then, we assessed the consistency between the two types of entry forms. Results showed a high consistency rate of 96.9%, with no inconsistencies identified in how patient conditions were recorded on the two different types of entry forms. Likewise, we did not detect any inconsistencies due to system-related errors. The hospital therefore decided to proceed with implementation of ePRO based on the electronic self-care entry form. However, we felt the self-made form was too simplified and lacked potential that could be developed further. This is when we first learned about Welby’s “My Carte ONC,” which we first implemented in May 2020 to make observational studies, and then in November 2020, to use in clinical practice.
Sagara Hospital in Kagoshima City is Japan’s only designated cancer hospital specializing in breast cancer. It is equipped with 80 hospital heads, including those for palliative care, and holds a track record of 695 breast cancer surgeries and 4,609 pre-/post-operative chemotherapy treatments in 2020. Just under 400 new patients started chemotherapy in 2020, and about 60% of them reside in remote areas or on remote islands.
The hospital recognized the need to strengthen measures for managing adverse reactions for multiple reasons. Firstly, the facilities within the prefecture offering anti-cancer treatment concentrate chiefly on central areas, and treatment of adverse events for patients living in remote areas or on remote islands is often delayed, or treatment in general cannot be managed in terms of effectiveness due to remote geographical locations. Secondly, immune checkpoint inhibitors (ICI) became available for patients with breast cancer last year, and subsequently, cases that require immune-related adverse reaction (irAE) management have increased. Further, patients in general were refraining from visiting hospitals due to the COVID-19 pandemic. Amid such circumstances, timely information sharing between doctors and patients was key to offering safe out-patient chemotherapy. We realized that ePRO had potential to help resolve the issues we were struggling with and began preparation for implementation.
Track record of ePRO implementation over the year
As far as how we implemented the ePRO app, we initially started by transitioning print-based patient-reported outcome (PRO) to ePRO for patients accustomed to using smartphones, as part of measures for managing adverse events in pharmacotherapy cases. We asked patients to install the app on their own smartphones. When it came time for doctors to explain pharmacotherapy to their patients, they introduced ePRO as a measure for managing adverse reactions. Nurses played a key role in helping patients understand how to install and operate the app, using explanatory brochures. Once doctors and nurses at the chemotherapy center confirmed that the app had been properly installed, study participant IDs were registered to enable connection with the hospital’s system. ePRO was now ready for use.
Currently, nurses in charge of the chemotherapy room and Oncology Department doctors routinely confirm information entered by all registrants twice a day on weekdays. The app is designed so that when a grade 2 or higher adverse event is detected, it alerts users with easy-to-understand blue, yellow, and red visual keys to indicate the progression in grade. Our policy requires us to contact patients by phone if grade 3 or 4 and above adverse events are observed for consecutive days. Doctors view the information entered in the app by patients prior to medical consultations.
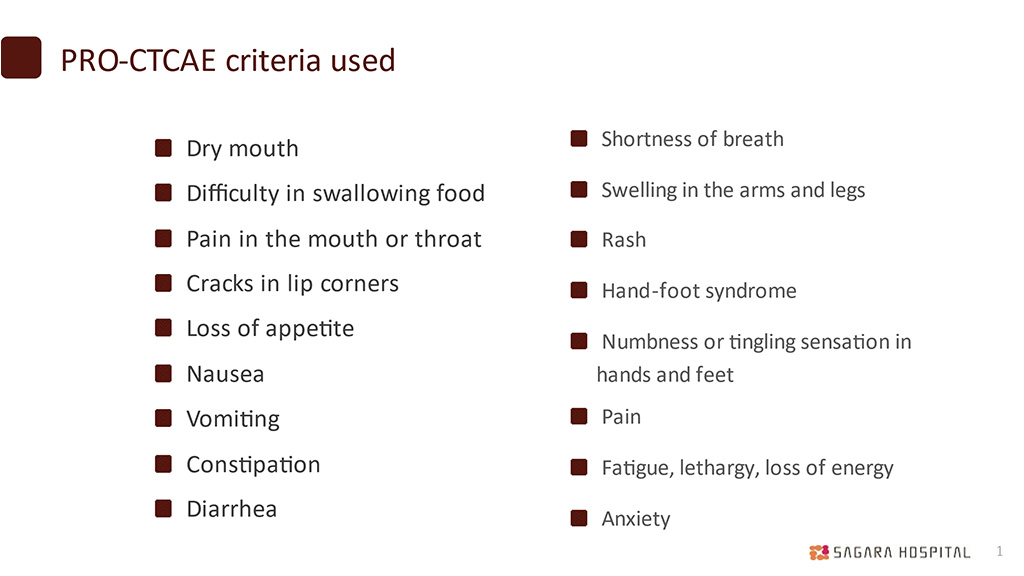
At the time of implementation, the rate of app registrants was more than 20 per month. Then, we noticed a slight drop in registrants, but it has now increased to 16 per month. Print-based forms are still used, and at this time more patients use the print form over the electronic version. However, the ratio of app registrants is finally beginning to increase. During the one-year period from May 2020, there were a total of 131 app registrants with a median age of 52 and a total of 262 print-based form users with a median age of 64. Reasons given for choosing the print form over the app include: preference for handwriting; dislike or unfamiliarity toward apps; not being able to download the app; and not knowing passwords. A median 84% of those who opted to use the app actually made entries during the required period. The 17 PRO-CTCAE criteria used are shown in the attached table. Additionally, during the one-year period, there were 18 cases in which we were alerted by ePRO and intervened via phone. The most frequent events were diarrhea (9 cases), followed by arthritis (7 cases), fever (5 cases), fatigue (5 cases), loss of appetite (3 cases), and peripheral neuropathy (3 cases).
Feedback on ePRO implementation
We conducted a survey on patients who used the app. The time it took to make a single entry in the app was 4.6 minutes on average and 1-3 minutes for the majority of patients. Among all users, 62.9% patients responded that the system helped them to convey adverse reactions to healthcare providers. Among those who switched from the print-based form, 87.5% felt that making entries in the app was better than filling in the print-based forms, 85.7% felt they were less likely to forget making entries with the app, and 85.7% wished to continue using the app.
We also collected feedback on user-friendliness: “Since making entries on mobile phones was very easy, I would like to use [the app] for my own personal record as well”; “One can feel a sense of security being connected to the hospital”; “I was grateful to receive a phone call from a nurse when I wasn’t feeling well”; “It was easy to record, organize, and summarize my condition and adverse reactions”; “It was good to be able to reflect [on my condition] every day”; and “I felt that cancer information-related services were very beneficial.”
Suggestions from patients helped shed light on important areas to improve, including: “There were many questions that didn’t fit my adverse reactions”; “The questions were the same in every situation. If there were questions more relevant to the patient’s symptoms, it would be easier to check as appropriate and thus convey them”; “I would like a medical record that could be adjusted according to the type or timing of anti-cancer therapy”; “I’m not sure if [my entries were properly] communicated, since it wasn’t raised during medical exams”; and “If images can be shared with the permission of the [patient] user, it would be better because changes could be tracked more easily.”
From the healthcare provider perspective, the benefits of ePRO are numerous: 1. remote patient monitoring, as well as fostering a sense of security and trust between doctors and patients who live on remote islands or in remote areas, or those who have refrained from visiting the hospital because of the pandemic; 2. a reduction in adverse events attributable to timely care, thereby making it possible to maintain treatment strength, improve safety, and reduce risks of emergency hospitalization; 3. less time taken to assess adverse events by visualizing adverse reactions; and 4. a more convenient process of registering information on databases and a reduction in errors, thus improving the quality of the databases.
Lastly, one key area of improvement from the healthcare provider perspective is that it can be a challenge for elderly patients to use ePRO. Our plan, then, is to continue using print-based PRO while moving forward with efforts to expand ePRO use, in preparation for when the generation of current smartphone users begins to age and IT takes on a larger role in medical care. An additional challenge is that it is difficult for patients to get into the habit of making entries every day. We plan to adjust the required frequency of entries based on each patient’s therapy regimen or treatment cycle and the extent of adverse events. Further, to address the fact that patients experience symptoms and have concerns that are not covered by the questions, we plan to learn more about patients’ concerns when providing in-person care. We also plan to promote advanced care planning (ACP). We will also engage in activities to promote ePRO through study sessions or lectures in a hospital setting to address inadequacies in healthcare providers’ knowledge.
Presentation 2
Updates on research on the latest ePRO in the oncology area
Tempei Miyaji, Project Assistant Professor at the Department of Clinical Trial Data Management, Graduate School of Medicine, The University of Tokyo
The benefits of ePRO are garnering global attention
ePRO refers to the method of and system for the electronic collection of PRO. It was initially used as electronic data capture (EDC) in clinical research for eSource, but is now starting to gain attention for its potential use in symptom monitoring, self-management, patient and healthcare provider communication, and intervention in daily clinical practice. This trend was spurred by prior research conducted by Basch et al,* which was presented at the 2017 American Society of Clinical Oncology (ASCO) Annual Meeting. Since then, numerous additional studies, including feasibility studies and research projects on its potential implementation have been planned in various countries. In Japan as well, studies assessing the benefits of ePRO-based monitoring in patients with breast cancer have been conducted.
*In the study, patients receiving anti-cancer treatment were asked to record adverse reactions themselves once a week using digital tools such as PHR, and when adverse reactions of a certain grade or higher were recorded, interventions were made when necessary and as appropriate. Results showed that overall survival was extended by 5.2 months compared to patient groups that received routine care.
Overall survival results of a randomized trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment, Ethan Basch, MD, MSc et al, JAMA July 11, 2017 Volume 318, Number 2
Improving accuracy of symptom assessment by incorporating patient assessments
In everyday clinical practice, ePRO is used for: 1. PHR; 2. monitoring symptoms and alerting healthcare providers. The key benefits are: 1. improvement in the accuracy of symptom assessment; 2. enhancement of communication between healthcare providers and patients; and 3. maintaining QOL, reduction of emergency hospitalization or out-patient care, and prolonging survival. In terms of improving accuracy in symptom assessment, Basch’s 2010 research points out, “There is a disparity between healthcare providers’ assessments and patients’ voices. Healthcare providers tend to underestimate patients’ subjective symptoms, and assessments by healthcare providers alone is insufficient.” These insights prompted greater interest in incorporating patients’ voices using ePRO. Japanese research has also identified inconsistencies in assessments by healthcare providers and patients. In addition, some research has confirmed cases in which the accuracy of symptom assessment improved when print-based reports were switched to ePRO.
Problems using ePRO
The following is about a report on ePRO usability by PRO-TECT, a study conducted by Basch in the U.S. Patients who use ePRO were asked about their experience three months after their first use. About 90% responded that the questions were easy to understand; the system was easy to use; and the questions were relevant to them. While 70% agreed that communication with doctors and nurses improved, stating that their doctors and nurses actually used the data, 30% did not agree and felt that there was room for improvement. Seventy percent believed ePRO was beneficial to patients’ self-management, and 90% agreed that they would recommend it to others.
Similarly, when nurses were questioned after three months of use, about 80% responded that ePRO was beneficial in human epidermal growth factor receptor (HER) records; communication with patients improved; and efficiency levels improved. Meanwhile, only about 60% agreed that the quality of patient care improved; that they would use the same system for patients in the future; and that they would recommend the system to other clinics. These results revealed that there are more medical professionals than patients who do not fully appreciate the benefits of ePRO.
Further, feasibility studies on elderly patients are underway as well. In research that examined entries by patients with bladder cancer aged 68 on average, 70% of the patients made entries until the fifth cycle, while a relatively lower portion of healthcare providers checked the data. This study also affirms that although there appear to be no problems with use among the elderly population, healthcare providers are not making full use of it.
Developing implementation strategies in light of inhibitors and success factors
We also had the opportunity to gain insight into research results on inhibitors and success factors when ePRO is implemented in everyday clinical practice. Issues with inhibitors include: 1. technical problems (related to devices, network, or linking to electronic medical records); 2. the lack of knowledge and awareness of PRO among parties involved; 3. ambiguity in how and why PRO is collected; 4. negative effects (increase in workload, decrease in satisfaction toward patient care); 5. conflict with requirements of established daily operational processes. On the other hand, numerous success factors were also observed: 1. the ability for each medical institution to make operational adjustments; 2. the ability for key people at each medical institution to make adjustments; 3. relatively easy operation of ePRO itself. Based on this information, we believe that ePRO implementation strategy could go as follows as: 1. [before implementation] communicate with all parties involved, and enhance understanding of ePRO’s benefits, as well as assess and coordinate operational flows; 2. [during implementation] provide training and support to staff for whom ePRO is a potential burden; and 3. [after implementation] follow-up and manage problems that arise.
Challenges in ePRO implementation and future use
What we know now – key learnings
- -Clarify assessment criteria and limit alerts (to alleviate burden on both patients and healthcare providers).
- -Set thresholds in alerts.
- -Visualize viewers and create reports.
- -Link to electronic medical records (coordinate with medical information divisions or electronic medical record vendors). This agenda item is related to security policies and most likely needs to be resolved in terms of stakeholder management.
- -Examine how ePRO assessment and PRO data references can be translated to everyday operational flows at clinical sites.
I look forward to seeing research advance even further to resolve such issues. At the same time, I do believe that all relevant parties need to consider how to work together to successfully implement ePRO.
Lastly, some final thoughts on the future of ePRO.
- We can expect more results of studies on ePRO implementation in everyday clinical practice both in and outside of Japan.
- PRO-CTCAE is expected to become the mainstream ePRO-based adverse event assessment tool for cancer in Japan as well.
- As ePRO is more widely implemented in daily healthcare settings, we can expect to see multiple models being developed according to organizational scale or subject users.
- Linking ePRO with electronic medical records is likely to progress gradually in phases.
- Going forward, ePRO will advance not on its own but in combination with online healthcare, mobile heath (mHealth) technologies, and patient portals.
The webinar concluded with a lively panel discussion and Q&A session entitled “Issues and potentials of digital tool usage in patient disease management.” Joining Tetsuhiko Taira and Tempei Miyaji were Reiko Makihara, a pharmacist specializing in cancer at the Department of Pharmacy, National Cancer Center Hospital, and Naomi Sakurai, Cancer Survivors Recruiting Project, who facilitated the discussion. Click here to access the video of the session (Japanese language only).