More than a year has passed since the COVID-19 pandemic began. Among the many consequences being felt by us all, one issue that stands out is the impact on operations at public health centers, a body that tended to garner little attention in the past. The past year has underscored the important role public health centers play, but has also shone a light on the difficulties created when such centers are forced to focus exclusively on one disease, in this case COVID-19.
For this issue of the COSMO Newsletter, we wanted to understand how this situation is particularly affecting HIV transmission and treatment. We sat down with guest contributor Kota Iwahashi, President of akta, a non-profit organization that offers education and support to those affected by HIV and AIDS, to gain insights into the latest developments when it comes to HIV transmission in and outside of Japan.
The following guest contribution is compiled from an interview with Kota Iwahashi, President of akta, conducted exclusively for COSMO Newsletter readers.
 Kota Iwahashi
Kota Iwahashi
President, akta
1. HIV infection and AIDS in Japan today
More than 80% of HIV-positive patients attributed to male-to-male sexual contact
According to a pre-pandemic report in 2019 by the Ministry of Health, Labour and Welfare’s National AIDS Surveillance Committee, there were a total of 1,236 patients in Japan who were HIV-positive or diagnosed with AIDS. The report also supports two notable trends of HIV infection in Japan. Firstly, around 67% of patients (831) were infected through sexual contact between Japanese nationality males, and secondly, 33% of cases (406) were reported in Tokyo. However, actual transmission routes often differ from that reported by the patients themselves. Physicians treating HIV infections estimate that in fact more than 80% of infections in Japan are due to male-to-male sexual contact.
HIV testing significantly down due to COVID-19
COVID-19’s biggest impact on anti-HIV efforts is the drop in HIV testing. In Japan, the most accessible HIV tests are those offered anonymously and free of charge at public health centers nationwide. However, when these centers became key sites for tackling COVID-19, they could no longer provide HIV testing. Quarterly reports from national public health centers confirm that the number of HIV tests performed drastically fell in Q1 and Q2 of 2020, corresponding with the pandemic’s timeline. Similar trends have also been noted in the past when novel influenzas or the Great East Japan Earthquake struck Japan, but the extent of the decline this time is at an incomparable level.
Efforts to tackle COVID-19 efforts are of course critical, but it should not be forgotten that HIV infection and other sexually transmitted diseases continue to affect society. With the spread of vaccination, the COVID-19 pandemic may come to an end, but if this lack of opportunities to receive HIV tests within communities continues, we may see an increase in patients who only discover their HIV-positive status after AIDS has manifested. It’s a critical issue in terms of prevention, early detection, early-stage treatment, and prognosis of HIV infection. How can we accommodate the needs of those who seek HIV tests? The situation not only poses practical problems for those offering HIV tests, but also the broader important issue of how we evaluate citizens’ rights to receive health tests.
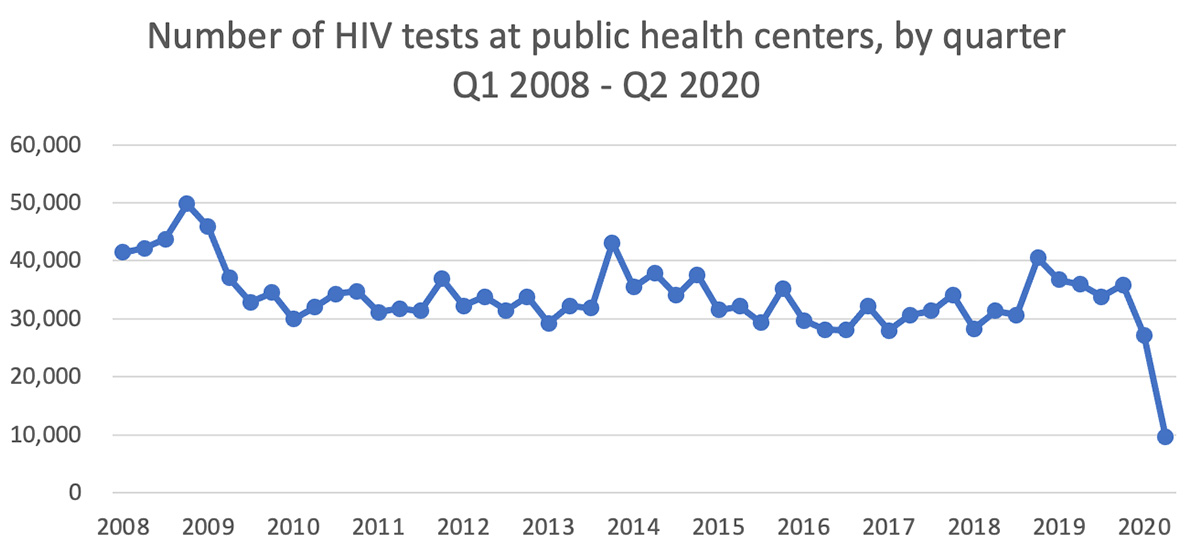
Source: 155th National AIDS Surveillance Committee
The need to secure different routes to testing
In the UK, where the pandemic is considered to have taken a greater toll than in Japan, the effect on HIV testing has been temporary and less extensive. Some attribute this to UK having taken efforts to diversify testing routes through initiatives such as postal testing, tests performed at local clinics, or implementing new methods such as self-testing (ST). Moreover, encouraged by the British public’s growing interest in infectious diseases, the TV series ‘Its’ a Sin’ was aired, depicting the stories of HIV-affected gay communities in the 1980s. The popularity of the series saw HIV testing rates during the campaign period increase fourfold over the previous year.
Why are postal HIV tests still uncommon in Japan? Healthcare systems around the world have been struggling with remote health tests, or tests that do not require users to visit public health centers or clinics. The quality of such tests is not assured so postal tests are only for screening purposes and require users to initiate all the subsequent steps on their own, including definitive testing or treatment at medical facilities. Moreover, a considerable rate of postal tests in Japan are made collectively in groups, posing potential privacy issues. For example, sex workers often receive tests according to the organization they work for, and test results are often sent to the organization instead of the individual. In addition to tests offered at public health centers and testing facilities nationwide, new means of testing need to be developed at scale. In this sense, COVID-19 has brought about a timely opportunity to reconsider the status quo.
HIV test strategies for MSM under COVID-19
HIV testing at public health centers will always remain crucial, but in light of these many issues, including the current inability to offer testing during the pandemic, restricted operating hours, and an aversion among men who have sex with men (MSM) toward in-person testing, we at akta set about to actively address the need to secure new testing opportunities outside beyond those at public health centers and discussed a strategy to support MSM during the pandemic.
The strategy identifies postal tests and private-sector medical care (clinics) as alternative routes to testing and proposes ways to effectively encourage their usage including: (1) having community centers, NGOs, and NPOs use smartphone apps to conduct campaigns to reach MSM and promote these testing methods; (2) engaging the government from an early stage; and (3) collaborating with key figures in respective communities’ medical care systems and strengthening ties with local clinics.
Prior to this, akta, where I serve as president, handed out a test kit called “HIV check.” The project was a success with 82% usage rate among those who received a kit during the 18-month period until the end of January 2020. Of these, 3.82% were found to be HIV-positive. This happened before the pandemic but nonetheless confirmed the benefit of having community centers take a central role in offering testing opportunities.*
Building on this experience, we set out from FY2020 on a new endeavor, bringing together nine communities across Japan to form the ‘MSM All Japan Team’ to distribute postal HIV and syphilis test kits to MSM as part of a pilot project within the Ministry of Health, Labour and Welfare’s research framework.
*Click here for more details on akta’s activities.

Banner introducing the postal HIV and syphilis test kit project
2. Advancing HIV and AIDS measures worldwide
The “combination prevention” approach
The global community’s awareness of and efforts for HIV and AIDS are significantly changing. UNAIDS (Joined United Nations Programme on HIV/ADIS) has “ending AIDS” as its slogan with a vision of ending the AIDS epidemic as a threat to public health by 2030. The choice of using the words “ending AIDS” instead of “stopping AIDS” is a deliberate one; the program aims to help build a world where HIV-positive people can also live long, healthy lives, rather than a world where AIDS and HIV-positive people don’t exist.
To achieve this, UNAIDS advocates the “combination prevention” approach, which is defined as minimizing new infections by taking preventive measures suitable at a particular point in time, using means that combine different tools and methods found in behavioral sciences-based, bio-medicinal, and structural strategies. This approach is about selecting the most optimal HIV prevention methods from a tool box of possible options and is founded on the principle of human respect for all, particularly pertinent in light of recent trends affecting respective communities.
The “U=U” message

A key factor in promoting the combination prevention approach has been the “U=U” message. Owing to the spread of highly effective HIV treatment and the steady accumulation of international research-based evidence, it has been scientifically proven that if the HIV virus is undetectable, or is controlled to a level below the detection threshold, it is untransmittable and cannot infect others, even when HIV-positive people have sexual intercourse. “U=U” has become a new common understanding and bears great significance for people living with HIV. The Japanese Society for AIDS Research has also been quick to support campaigns based on the concept.
PrEP as a game-changing option
Another important option in combination prevention is PrEP (pre-exposure prophylaxis), a procedure in which HIV-negative people take anti-retroviral therapies to prevent infection. The US Centers for Disease Control and Prevention (CDC) announced guidelines on recommendations for the procedure in 2014, followed by WHO.
Access to PrEP is limited to those at risk of HIV infection. Condoms remain essential for preventing infection, but when they cannot be used, PrEP is another option. Its availability is a key part of the combination prevention approach but unfortunately, although such anti-retroviral therapies have been used for a long time for the treatment of AIDS, they are not approved for preventive purposes in Japan. In fact, Japan is the only country in East Asia that has not approved PrEP.
Of course, risks surrounding the “U=U” message and option of PrEP need to be considered. For example, the spread of PrEP has seen a fall in condom use, triggering a rise in other sexually transmitted diseases such as syphilis in some communities. Going forward, it will be important to advocate combination prevention and increase medical care options. That said, we still need to address the new agenda of developing “health literacy” among communities, and individual’s ability to independently obtain accurate information and properly understand it.
3. New international targets
2020 goal: 90-90-90 Target

Source:UNAIDS 90–90–90 – An ambitious treatment target to help end the AIDS epidemic
To achieve the afore-mentioned goal of ending the AIDS epidemic as a threat to public health by 2030, UNAIDS established the interim “90-90-90 Target” in 2014, calling for 90% achievement of three goals. Specifically, achieving the following by 2020: (1) 90% of HIV-positive people are aware of their own infection; (2) 90% of those aware of their infection receive anti-retroviral therapies; and (3) 90% of those receiving treatment have their viral load controlled below the detection threshold.
2025 AIDS Target: Putting people at the center
Unfortunately, assessments in 2020 concluded that the 90-90-90 Target had not been achieved globally. In response, UNAIDS established a new 2025 AIDS Target as a five-year interim target, also taking into account experienced gained from COVID-19, as announced in its World AIDS Day 2020 report: Prevailing Against Pandemics by Putting People at the Centre.
Importantly, this approach centers around people living with HIV and communities exposed to high levels of HIV infection risks. It puts forth indicators, such as the six “95%’s” to address three areas of provision of holistic services, integration of services that meet respective circumstances, and elimination of social and legal barriers that inhibit service availability.
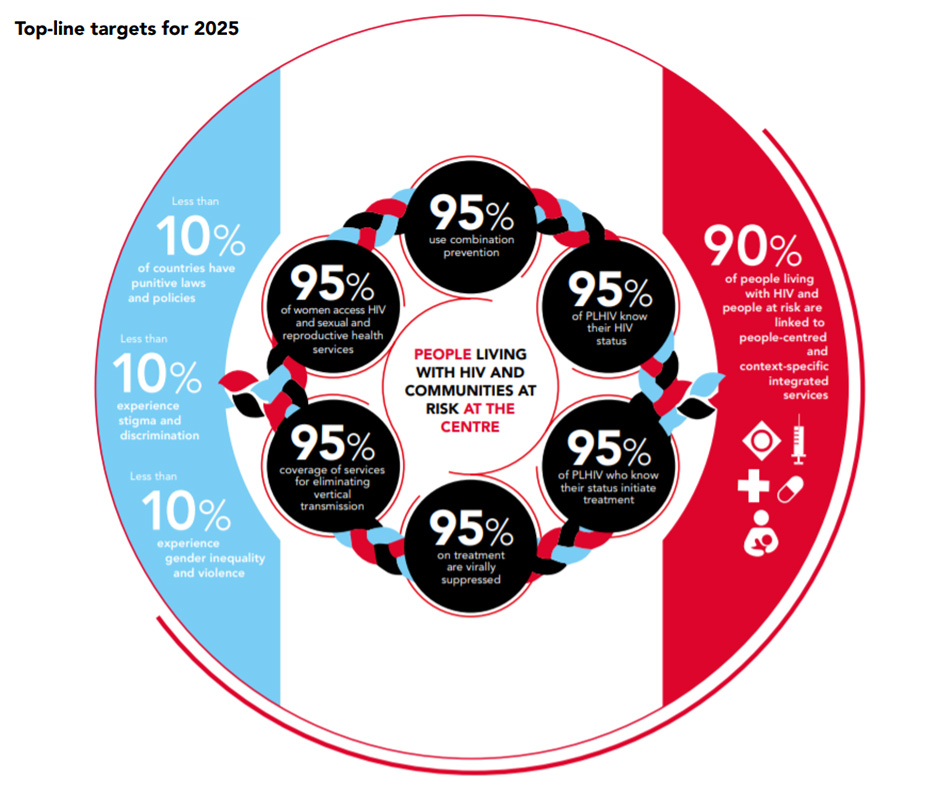
Source: Prevailing Against Pandemics by Putting People at the Centre (World AIDS Day 2020 report)
Winnie Byanyima, Executive Director of UNAIDS, comments, “These targets are centered around people at high risk of HIV infection or pandemics such as COVID-19 who tend to be isolated from society. They aim to resolve inequalities that aggravate the spread of pandemics,” underlining the importance of people-centric approaches with societal and community support. Such a concept offers a good basis of thought when Japan reflects on its past HIV measures and considers its future policies NGO activities.
4. Closing remarks
I have discussed how the situation surrounding anti-HIV efforts is evolving and significantly changing, but unfortunately, interest toward HIV is diminishing, and the level of awareness of HIV remains low among general society. According to results of the Cabinet Office’s Survey on Awareness of HIV Infections and AIDS in 2018, 52.1% still believe that AIDS is a fatal disease, and 33.6% believe that the disease arises from unknown causes and has no effective treatment.
Meanwhile, with respect to the latest information on HIV and AIDs, 33.3% are aware of the fact that risks of infecting others can be reduced, 26.5% understand that HIV-positive people can enjoy a close-to-average life expectancy with proper treatment, and 35.1% do not know of latest information, scoring the highest.
If we are to close the gap between targets and reality, we urgently need to update the understanding of latest information on HIV and AIDS. Needless to say, NPOs and NGOs involved in the awareness-raising and education of HIV and AIDS need to continue driving this effort, but I also believe that this is something we, the society as a whole, including the education sector, need to engage in.
(Interview conducted on February 25, 2021 by COSMO Healthcare)